NEED TO KNOW
- A Northern California mother, Jessica Farwell, recalled how she was charged over $100,000 for a visit to the emergency room
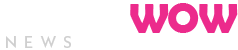
- In October 2022, her son, Brody, suffered second-degree burns from a rice cooker
- After the worried mother drove him to the local hospital, he was transported to the nearest burn unit, resulting in the six-figure hospital bill
A mother is recalling how an emergency room visit for her newborn baby resulted in a six-figure hospital bill.
Jessica Farwell, a resident of Antioch, Calif., told KGO-TV that in October 2022, a rice cooker fell off her kitchen counter and severely burned her infant son, Brody, who was 6 months old at the time.
“His skin, it just instantly bubbled up,” she began. “I was just like — is his face going to start bubbling?”
The worried mother then rushed her infant to the nearby hospital, where “they gave him fentanyl through his nose because he was screaming.”
However, the facility lacked a burn unit and had no ambulances to transport Brody to a hospital with a burn unit. “So they were calling an ambulance, but it was the end of COVID. There wasn’t going to be an ambulance for seven hours,” she explained.
It was then declared it was medically necessary to transfer Brody to Shriners Children’s Hospital in Sacramento. (Antioch is 58 miles south of Sacramento.) To bypass the seven-hour wait for an ambulance, she offered to make the one-hour and 20-minute drive.
“They said, ‘No, sorry, you can’t — I can’t let you leave with him. I’ve already called the helicopter.’ He basically told me there was nothing I could do,” Farwell explained.
That’s when she was presented with the sole option of a 15-minute helicopter ride that cost nearly $90,000 — while being reassured, she told KGO-TV, that she would not receive the bill since the hospital requested the helicopter and she had insurance.
“I was just absolutely terrified to fly — I’m breaking down. He’s screaming; it was just awful,” she said.
Yet, when they landed at the burn unit’s helipad, she was informed that an ambulance ride was required to take them to the hospital entrance, only 0.3 miles away.
“You can see the hospital,” Farwell told KGO-TV of the location where they landed. “You literally can walk across the street to the hospital quicker than that ambulance, and they charged me $10,200.”
Upon their arrival at the burn unit, her son was treated for his second-degree burns and discharged the next day.
However, Farwell wasn’t finished with the experience. A couple of months later, she received the bill for $100,032.
“I couldn’t believe my eyes,” Farwell said. “You look at the bills, and it’s absolutely enraging. We got hit for a $600 waiting fee; there’s a fee for it being a nighttime service. There’s just every single fee you can think of.”
Although the doctors said the bill wouldn’t be an issue because of her insurance, she learned that insurance only covered less than half of the helicopter bill and a small portion of the ambulance bill. She was then left to cover $57,929.80 for the helicopter and another $7,327 for the ambulance.
“I’ve called the hospital, ambulance company, my insurance numerous times,” she said. “It’s been three years, and then they wouldn’t listen to me or talk to me. They just kept giving me the runaround.”
Never miss a story — sign up for PEOPLE’s free daily newsletter to stay up-to-date on the best of what PEOPLE has to offer, from celebrity news to compelling human interest stories.
After receiving ongoing calls from collection companies, which led her to search for help on Google, she found KGO-TV, who assisted her and ultimately had the entire bill waived.
“They called, and said, ‘It’s done, we will never bill you again.’ They almost sounded apologetic. I hung up and told my husband. We just couldn’t believe it!” Farwell recounted. “It’s a miracle!”
In January 2024, California passed the law AB 716, which protects people from receiving surprise bills for ground ambulance services. Since Farwell’s incident happened before the law was passed, her ambulance bill was not waived.
Ambulance company Pro Transport-1 told KGO-TV that they felt the “issue still 100% lies with the insurance company simply deciding to pass part of the bill to the patient, we will accept their partial payment and no longer seek the remaining balance of the bill for our services.”
When KGO-TV reached out to Blue Cross Blue Shield, the insurer said it could not answer specific questions about Farwell’s case, adding, “We are committed to increasing access to safe, appropriate, and effective health care based on the best available information and research, and in accordance with a member’s benefit plan.”
PEOPLE has reached out to Shriners Children’s Hospital and Blue Cross Blue Shield for comment.
Read the full article here